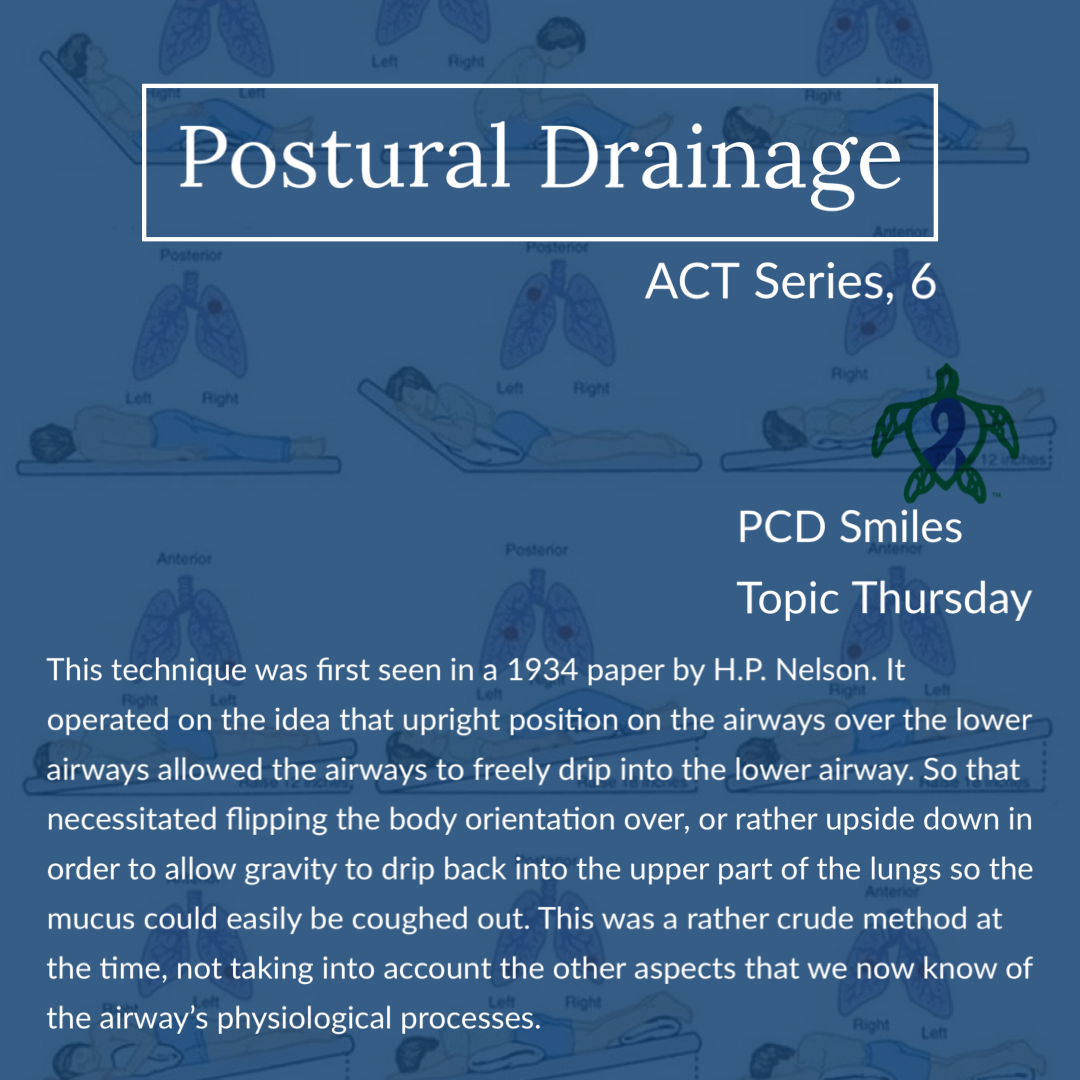
As the population who uses airway clearance techniques (ACTs) grows and ages with the advancement in pulmonary disease management, clinicians and patients alike are turning their attention to other airway clearance techniques. Advances in disease management of cystic fibrosis (CF) is allowing the CF population to age and as such clinicians and patients are starting to see things in these patient populations that were not an issue even a decade ago. Like CF patients going on to have children, careers, and so on. This has brought about the apparent need for more airway clearance techniques tailored for patient situational needs. Even both the internet and social media have played a huge role in making the world closer. Airway clearance techniques from around the world are now getting daily exposure to patients groups and communities that have never heard of them before. This has sparked huge controversy on which is the right ACT for each disease. Clinicians and patients in one part of the world have never been exposed to an ACT that is offered in another country. Instead they rely on limited studies from disease patient population on a particular ACT device or method. While an ACT device or method may work for idiopathic pulmonary fibrosis, that same device or method may not work or may even be harmful to cystic fibrosis patients or even PCD patients. It is very dangerous and misleading to say “device A” doesn’t work as well as “device B” for all pulmonary diseases just because a limited study on non-purulent pulmonary disease shows “device A” is not helpful to non-purulent pulmonary disease patients. The same could be said for a different ACT device that is successful at helping CF patients should in fact be the best device for asthmatic with pneumonia patients. The techniques for airway clearance are tailored towards certain physiological factors of the airways. Like certain ACTs target or rather help augment the cilia, and other ACTs target airway ventilation to aid in airway clearance.
Over the last sixteen weeks or so we have focused on the various types of airway clearance techniques, how they work, special considerations, contraindications, and if they can be standalone therapies or adjunct therapies to other ACTs. The biggest question(s) when it comes to airway clearance techniques that everyone wants to know is, which ACT is the best ACT? And which ACT is the best ACT for PCD (primary ciliary dyskinesia)? Overall no matter which disease it is, the best ACT is the ACT that the patient will actually do. That really is the key, because if the patient is not being compliant with their airway clearance therapy then what does it really matter which ACT is the best ACT?
When it comes to PCD the type of airway clearance technique that is best remains a big mystery due to very limited studies. On one hand you have the ACTs that target the cilia, ACTs with oscillation. Oscillation helps and aids cilia do their job by helping the cilia to beat faster. However oscillation therapy may not be appropriate for PCD where the cilia do not function properly. Think of it this way; if your car’s axle is broken and the wheels won’t turn and move the car, then it really does not matter how great and expensive the quality of gasoline is that you put in your car. Sure you can put the gas in, turn on the engine, rev the engine, but your car is still not going to move because the axle is still broken. Same is true with cilia in PCD. The cilia are missing their basic building blocks and applying oscillation to the cilia isn’t going to repair or replace the missing pieces of the building blocks that form cilia. Oscillation alone may not solely solve puzzle when it comes to ACTs in PCD care.
On the other hand ventilation airway clearance techniques may be the key to aiding PCD patients in maintaining their respiratory hygiene. This is because ACTs that rely on or rather use ventilation to assist in airway clearance therapy are not focusing on augmenting ciliary function. But rather it is airway ventilation that it being utilized to clear the airways. Ventilation can help get air behind stuck or plugged mucus and help to move the mucus along the peripheral airways to the central airways where it can be coughed out by the patient. ACTs that target ventilation also help to stent the airways open to prevent airway collapse as the mucus moves along the airways. Ventilation helps treat, resolve, and prevent atelectasis. Atelectasis is common clinical consequence of PCD due to the nature of PCD. ACTs that use both ventilation and oscillation may be the best combination for airway clearance therapy in the treatment of PCD. However there needs to be longitudinal studies into PCD airway clearance therapy to provide the best answers for PCD patients and their families. But unfortunately it is very unlikely that we will see any longitudinal data on airway clearance therapy in PCD, as the therapy focus has turned to gene modifier therapy. So for now, which ACT is the best ACT for PCD care will continue to remain a mystery. For more information on which airway clearance technique may be the best airway clearance technique for you or your PCD loved one ask your clinic’s licensed respiratory therapist or your clinic’s contracted respiratory therapy provider at your next visit.
While airway clearance techniques are widely used throughout the world; the physiological mechanisms and consequences of airway clearance techniques are mostly misunderstood in the context of the diseases that the airway clearance techniques are prescribed for. There are many considerations for airway clearance therapy Having medical professionals that are adequately trained on the specifics of airway clearance therapy, including everything we have discussed in our sixteen part series on ACTs; is a must for patient safety, including but not limited to the prescribing physician. Airway clearance techniques are intended to remove mucus from the peripheral airways to the central airways where the mucus can coughed out by the patient in a safe manner. The process of moving the mucus along the airways to be coughed out can last for several minutes after the treatment or rather ACT session has ended. Patients can expect to have increased voluntary and involuntary airway clearance, sometimes for several hours after the ACT session has ended. ACTs provide temporary increase in mucociliary clearance, which is why multiple ACT sessions are needed daily to be effective at helping maintain pulmonary hygiene or rather effective airway clearance.
A note of caution, it is important to remember that not all ACT devices and techniques are approved for use by patients or consumers by your regional regulatory agency. Great care should be taken when considering purchasing or using an ACT or ACT device available for sale on the internet, by unlicensed manufacturers including your neighborhood 3D printing guy, or even some device or technique being peddled by a social media influencer, life coach, or any person of the like. There are a ton of counterfeit ACT devices floating around out in the world of social media and the internet. Many of which can do serious harm to the person and their lungs. Be weary of even scientific looking literature claiming the device is a natural airway cleanser or detox device, or whatever the sales pitch is. In the context of PCD, always run any ACT or ACT device that you are interested in, or that someone else has told you about, by your PCD care team. It does not take much to damage delicate lung tissue, and permanent lung tissue damage is what we are trying to avoid for as long as possible in primary ciliary dyskinesia care.
Be sure to join us next week for another Topic Thursday.
Join our Facebook group Turtle Talk Café today.
We have several ways that you can donate to PCD Smiles;
- Visit Smile E. Turtle's Amazon Wishlist
- For more information on how you can donate, please visit our "Donation" page to check out our "Do & Don't policies.
- Or sponsor a PCD Smiles cheer package today!
- To shop for your “Official” turtle care ribbon gear today, visit PCD Style or Smile E. Cove
Thank you for your consideration!
***Please speak to your respiratory therapist or your PCD medical team before commencing any new treatment. DO NOT start using a device, or technique, on this website if you have not discussed this with your PCD team first.***