The United States PCD Foundation held its very first town hall meeting on 30 March, 2020 with one hundred and sixty nine attendees from the PCD patient groups. The virtual town hall panel consisted of North American primary ciliary dyskinesia experts Dr. Adam Shapiro of the Montreal Children’s Hospital, Montreal, Quebec Canada; Dr. Amjad Horani of the St. Louis Children’s Hospital, St. Louis, Missouri; Dr. Pamela McShane of the University of Texas Health Science Center, Tyler, Texas; and Anne Griffiths of the Children’s Minnesota, Minneapolis, Minnesota. The major theme of this virtual event was COVID-19 in the context of the PCD patient. The overall consensus of the panel was that the safest place for PCD patients and their immediate families is in their homes, unless the PCD patient needs respiratory support.
The virtual town hall got off to a start with introductions of the town hall panel members, who then took turns answering questions submitted by patients and their family members via the Zoom teleconference platform. There was a brief overview of the COVID-19 infection and its possible implications to the PCD population. To date there isn’t enough data that would indicate the potential of COVID-19 complications to the patient with PCD. The lung damage being seen post COVID-19 infection in recovered patients appears to be fibrosis like damage from the distinct type of pneumonia being seen with COVID-19 infections. Whether this will translate to lasting impact on post COVID-19 patients and their FEV1 scores remains to been seen. So far there are no known reported cases of COVID-19 in a patient with primary ciliary dyskinesia in North America today. To the panel’s knowledge this is true for Europe as well. The panel consensus was that this might be a good sign, but honestly there just isn’t enough relevant data at this point.
When pressed for recommendations for the PCD community, all panelists were in agreement that the patients need to limit contact until this event (pandemic) is over. Patients and their immediate family members should shelter in place for at least the next four weeks, with no one in or out of the home. If someone has to go for essentials, they should deliver essentials to the porch, clean and disinfect them, shower and change clothes, while washing the clothes they wore out. Patients and their families should avoid drinking and eating after one another. As well as avoid takeaway/take out and food not prepared inside the bubble of their own home. Take out poses a risk of infection from the food service industry employees and those that the employees comes into contact with. Patients and their families should severely limit the number of people who come and go from the home to virtually no one, including non-essential nursing services provided to the home. Stay in your bubble, stay in your homes, for at least the month of April and even the month of May. June and the months beyond June will have to be determined based on how the coronavirus ultimately unfolds in North America. Even once the peak of the virus has passed and various areas of North America start to lift their shelter in place orders, the PCD community will need to be very vigilant for at least the next twelve months or more. Prepare for things to stretch on and the possibility that the PCD community will be impacted by COVID-19 much longer than the general population. Remember there is no magic bullet for this. Well the magic bullet is actually to STAY HOME.
If your PCD family includes essential employees that must work, care must be taken to protect the PCD family member, including isolating them from others in the home. If the family member works in health care, that family member should not be performing duties that involve direct patient care. Performing clerical work from home instead is the best alternative for these families. PCD patients who work in the medical field should be working from home where possible or just not working. Families are encouraged to talk to their PCD care providers to obtain letters for employers to get work accommodations and or assistance.
The topic of shared parenting was brought up, and the general consensus was to limit travel between households for PCD children at this time. Shared parenting households are encouraged to work together to find solutions to limit their child’s exposure to as few people as possible. Keep their bubble small. This doesn’t mean that children should be kept from their other parent. But it does encourage parents to work together and find beneficial solutions to limit their child’s exposure to others. In researching this topic briefly, we’ve seen that this topic has been at the heart of several emergency court hearings. Even though most courts are currently closed or operating on emergent basis, court officers are holding virtual hearings to help parents navigate this unprecedented time. There are currently no States in the US who are granting a suspension of visitation rights solely because one parent is an essential employee or healthcare worker. The courts are suggesting that parents work together to limit an at risk child’s exposure to other people in the best interest of the child. And that the parent retaining custody in a shelter in place or quarantine situation makes extra effort to allow telecommunications with the other parent as often as necessary, and that after the limitations are lifted to grant extra visitations on a case by case basis. Parents in the above described situations should make every effort to work with one another and each other's attorney as needed.
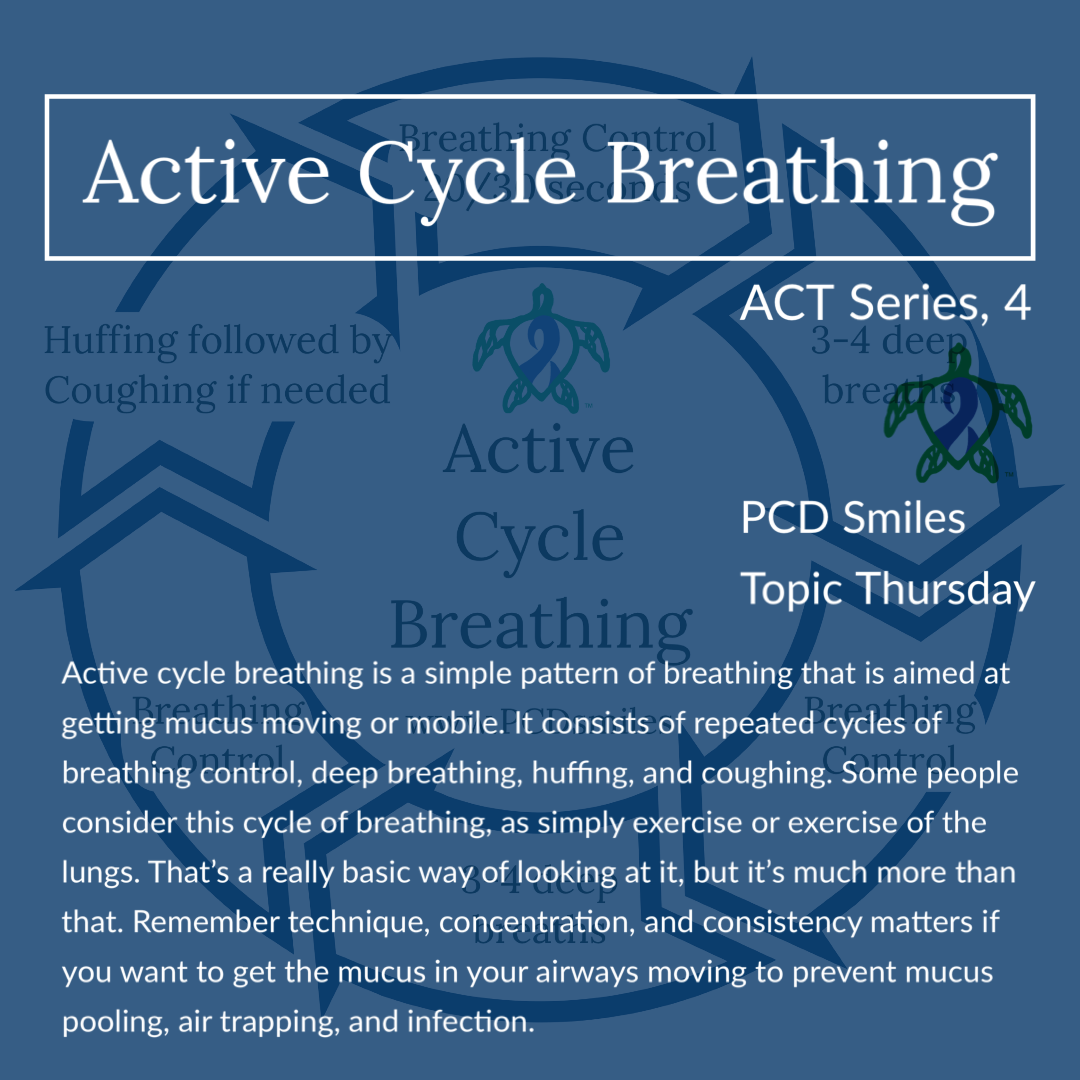
PCD patients are encouraged to continue all their therapies and not to discontinue anything or add anything without speaking directly to their care team. The panel members encouraged patients to keep up with their sleeping, eating, and exercising habits. This gives the PCD patient a good overall pulmonary edge or stamina if the PCD patient was to contract COVID-19. Patients should cough into a tissue, then bin it (throw it in the trash), and wash their hands. Each member of the panel said continuous hand washing is a must. Wipe down all surfaces, handles, and regularly clean the bathroom. There is indication that an infected person can shed the virus though their stool for a month or more. Sharing a bathroom with a suspected COVID-19 patient is not an option. Even people with mild illness can spread COVID-19 for many weeks. The panelist also said lightly wiping down delivered packages would be a good idea as well; although being overly obsessive about it is not necessary. PCD patients should treat all symptom flares as a PCD flare until the symptoms are proven otherwise.
PCD patients are encouraged to keep their stamina up and to stick with low risk activities. Now is not the time to end up in an emergency room with a broken limb. The emergency room is the last place a person with PCD needs to be right now. PCD patients should utilize all their protocols at home as much as possible. If your treatment protocols at home are not working contact your PCD team. It is important to note that any aerosolized treatment option can spread COVID-19 through the air if the patient receiving the aerosolized treatment is infected with COVID-19. It is for this very reason that almost no emergency room in North American is currently giving breathing treatments in the emergency rooms. Emergency rooms have switched to inhalers instead. COVID-19 patients are being treated, where possible, in zero pressurized rooms at facilities across North America. Individual facilities are working hard to come up with ways to give patients breathing treatments in their own facilities while at the same time protecting all other patients and medical personnel. If a PCD patient ends up hospitalized for non COVID-19 issues, their access to breathing treatments will most certainly be impacted. Stay home, your treatments are at home. This issue with aerosolization and COVID-19 will shape the way facilities handle breathing treatments, CPAP usage, BIPAP usage, and ventilator usage for the foreseeable future. Stay at home in your bubble, it is the safest place for a patient with primary ciliary dyskinesia. We are in this for the long haul North America.
Join our Facebook group Turtle Talk Café today, click here.
We have several ways that you can donate to PCD Smiles;
- Visit Smile E. Turtle's Amazon Wishlist
- For more information on how you can donate, please visit our "Donation" page to check out our "Do & Don't policies.
- Or sponsor a PCD Smiles cheer package today!
- To shop for your “Official” turtle care ribbon gear today, visit PCD Style or Smile E. Cove
Thank you for your consideration!