As we continue our deep dive into airway clearance our second, most basic, and next easiest airway clearance technique (ACT) is breathing. Breathing is another important part to all other airway clearance techniques. Breathing helps to get air in behind sections to help on the exhale to shear mucus with typical viscosity away from typical airway walls. The thicker the viscosity of the mucus the harder it is to shear the mucus away from typical airway walls with breathing and coughing alone. The same can be said for mucus that has less viscosity than typical mucus. Or rather if the mucus is too thin, thin mucus can prevent air from staying behind the mucus to allow for the exhale or expiratory forces of air to mobilize and move the mucus. In fact; if mucus is too thin, it can slip further into the alveoli area of the lungs where it gets stuck without more aggressive airway clearance measures. The condition of a patient’s airway walls also has some to do with cough and breathing to move mucus within the airways. But breathing for airway clearance is not your normal everyday breathing, it is breathing focused and directed with a purpose. It requires thought and concentration. This type of breathing for airway clearance is termed active cycle breathing or active cycle of breath in countries outside of the United States.
Active cycle breathing along with coughing is touted in most countries outside the U.S. as the premier of airway clearance techniques. They are the most prescribed ACTs out there and by far the cheapest' because they are free and everyone should be able to do them. Should being the operative word here. Whether coughing and breathing are effective ACTs for certain respiratory diseases is a topic of great debate for numerous reasons. This ranges from cost versus benefits analysis, patient cooperation, patient abilities considering their overall health picture, guidance of the medical regulatory agencies, care coverage, availability, knowledge, patient continuing education, country’s own research, and yes even patient satisfaction. Outside the U.S. patients are routinely given education counseling on breathing and coughing techniques. Inside the U.S. it may seem like these educational opportunities have fallen by the wayside for ACTs to the observer, but coughing and active cycle breathing are a big part of the larger or more complex ACTs available to these patients. Basically the way you breathe and cough during other airway clearance techniques does in-fact matter. Matter so much so, that not paying attention to your coughing and breathing while doing more aggressive techniques can basically mean that you are wasting your time. The same can be said for both coughing and active cycle breathing. If you are not doing them properly, they are not going to mobilize mucus. So then becomes the question of, “Why do ACTs at all then?” And on some concession; some pulmonary providers in the U.S. do gloss over breathing and coughing techniques during other ACTs without emphasizing the importance of proper breathing and coughing during ACTs. This is something that needs more attention in the world of respiratory therapy worldwide. In any case every country has it’s own opinion on what ACT is best for what pulmonary disease. What does seem to be the consensus is that the best airway clearance technique for a patient is the one that the patient will actually do. So what exactly is breathing for airway clearance then?
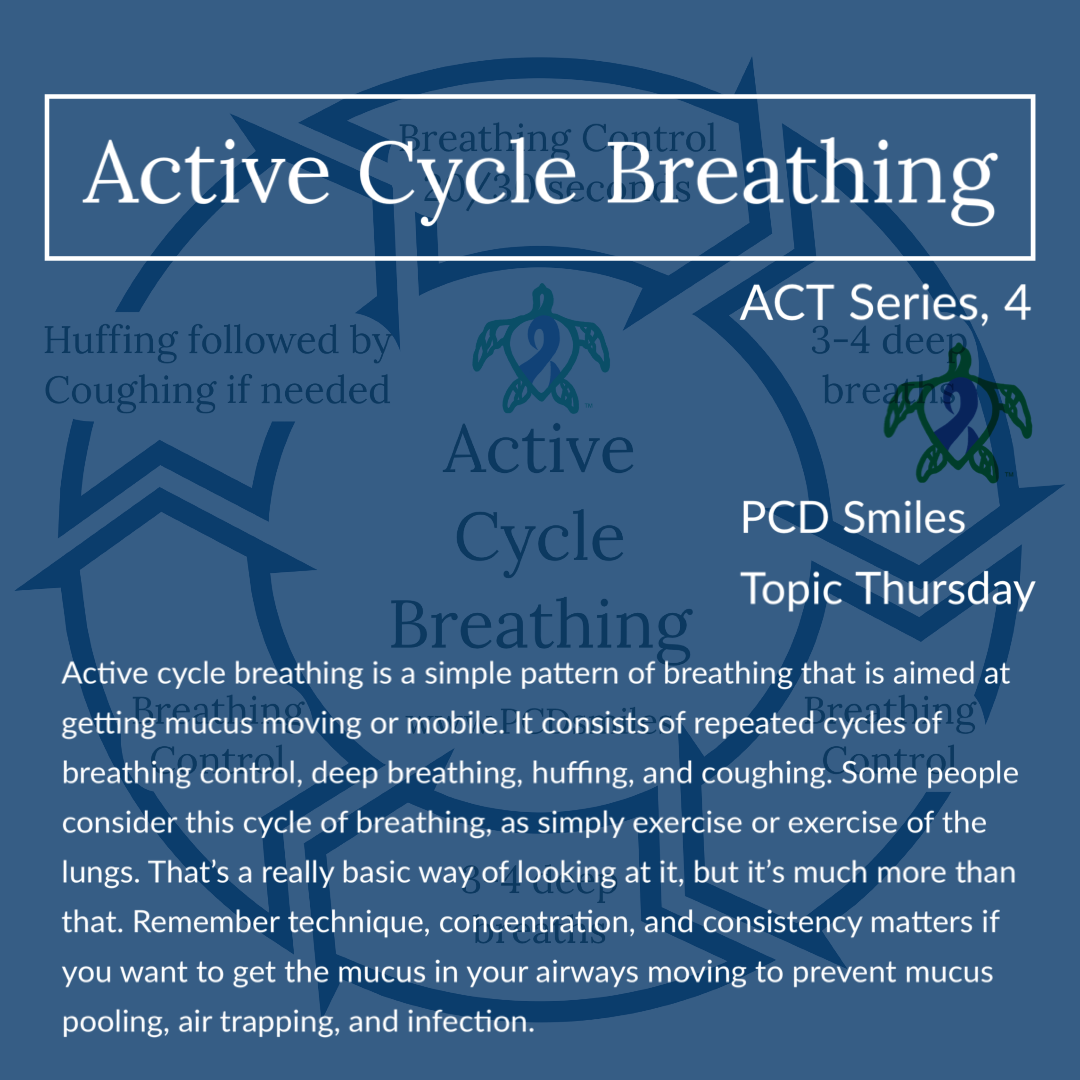
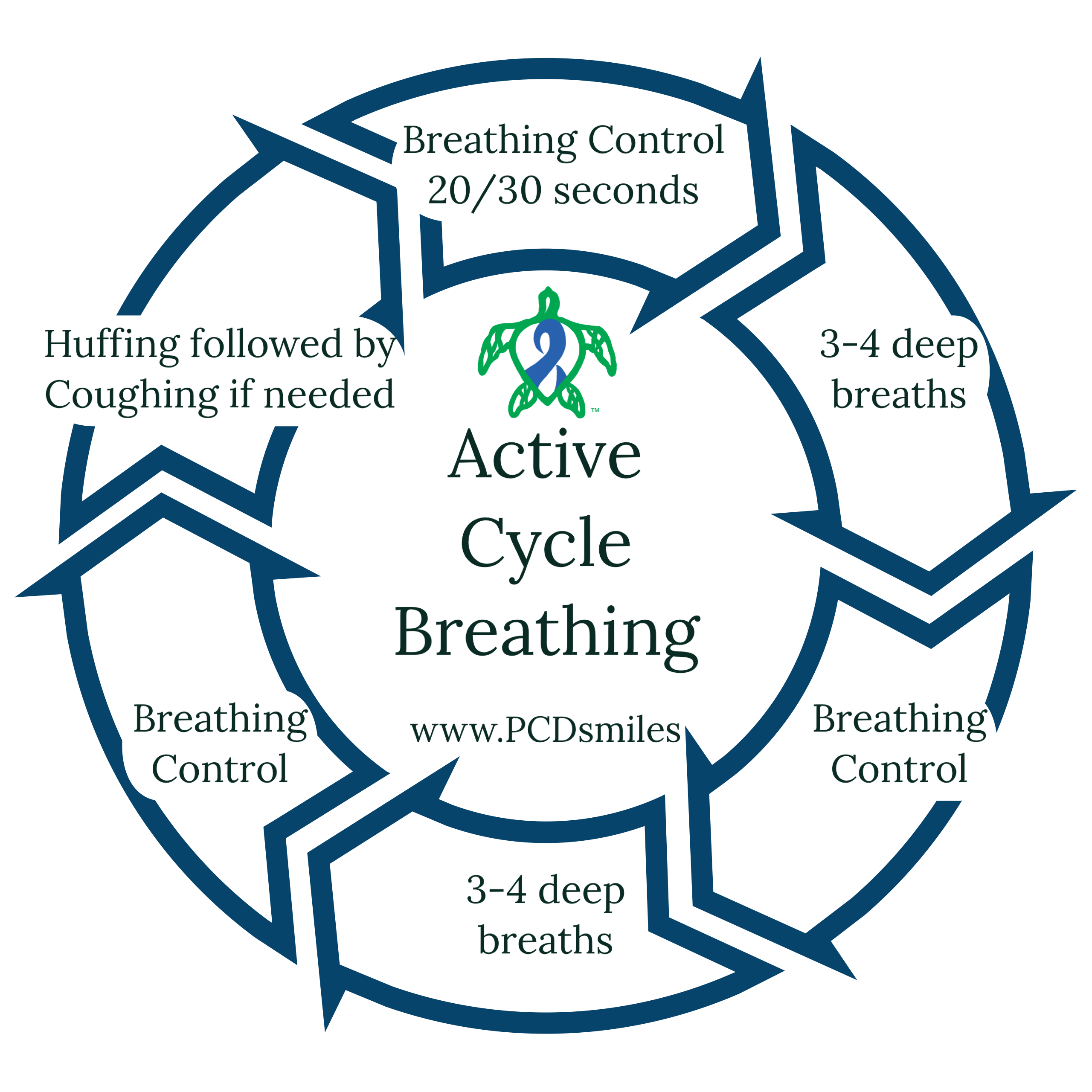
Active cycle breathing is a simple pattern of breathing that is aimed at getting mucus moving or mobile. It consists of repeated cycles of breathing control, deep breathing, huffing, and coughing. Some people consider this cycle of breathing, as simply exercise or exercise of the lungs. That’s a really basic way of looking at it, but it’s much more than that. Remember technique, concentration, and consistency matters if you want to get the mucus in your airways moving to prevent mucus pooling, air trapping, and infection. Once you learn proper technique of active cycle breathing you can then begin to apply it to other more aggressive forms airway clearance techniques like the airway clearance vests or PEP and OPEP devices.
Active Cycle Breathing (ACBT):
Adapted and sourced from Active Cycle of Breathing Technique - A Patient’s Guide
Find a comfortable position seated in an upright position, or whatever position that your other airway clearance technique requires (like one of the many autogenic drainage positions.) try to stay relaxed
Breathing Control
- Breathing gently using as little effort as possible.
- Rest a hand on your stomach and relax your shoulders.
- Breathe in and out quietly and gently, through your nose if possible.
- It is important to do this in between the more active exercises of ACBT as it allows your airways to relax.
Deep Breathing
- Breathe in through your nose slowly and deeply, keeping your shoulders and chest relaxed.
- Hold the breath for 2-3 seconds.
- Breathe out gently through your mouth.
- Repeat this up to 5 times; follow the advice of your respiratory therapist.
Huffing
- Breathe out (exhaling) through an open mouth and throat and not coughing.
- Squeezing air out through your open throat and mouth as if steaming up a mirror.
- Always follow huffing by breathing control.
Coughing
- If you can clear your mucus by huffing then you do not need to cough.
- Only cough if mucus can be cleared easily.
- After three coughs return to the beginning of the cycle with breathing control.
*Repeat the cycle until you feel that your huff or cough is not producing any mucus, or for up to twenty minutes depending on your respiratory therapist.
It was once thought in primary ciliary dyskinesia that coughing and breathing techniques like active cycle breathing were enough to compensate for the lack of mucociliary clearance seen in PCD. Recent research has now shown not only is this not the case, but that there is a sensory component to motile cilia. When motile cilia are under stress they signal the CFTR channel to do it's job and send more hydration to the mucus to thin the mucus in the airways. With defective motile cilia in PCD the CFTR never gets the signal, because the cilia are broken at the cellular level, which is thought why mucus viscosity seen in PCD is similar to that of the mucus viscosity seen in cystic fibrosis (CF). This could highlight why more aggressive airway clearance techniques are needed in PCD, especially as the destruction caused by PCD progresses. With some people with PCD needing aggressive ACTs in infancy. In any case as research in PCD advances, so will our understanding of cilia and it’s roles in clearing the airway. Learning the ins and outs of airway clearance techniques will remain an essential part of doing life with primary ciliary dyskinesia. We hope that you join us next week for part five of our series on airway clearance techniques.
Be sure to join us next week for another Topic Thursday.
Join our Facebook group Turtle Talk Café today, click here.
We have several ways that you can donate to PCD Smiles;
- Visit Smile E. Turtle's Amazon Wishlist
- For more information on how you can donate, please visit our "Donation" page to check out our "Do & Don't policies.
- Or sponsor a PCD Smiles cheer package today!
- To shop for your “Official” turtle care ribbon gear today, visit PCD Style or Smile E. Cove
Thank you for your consideration!
***Please speak to your respiratory therapist or your PCD medical team before commencing any new treatment. DO NOT start using a device, or technique, on this website if you have not discussed this with your PCD team first.***