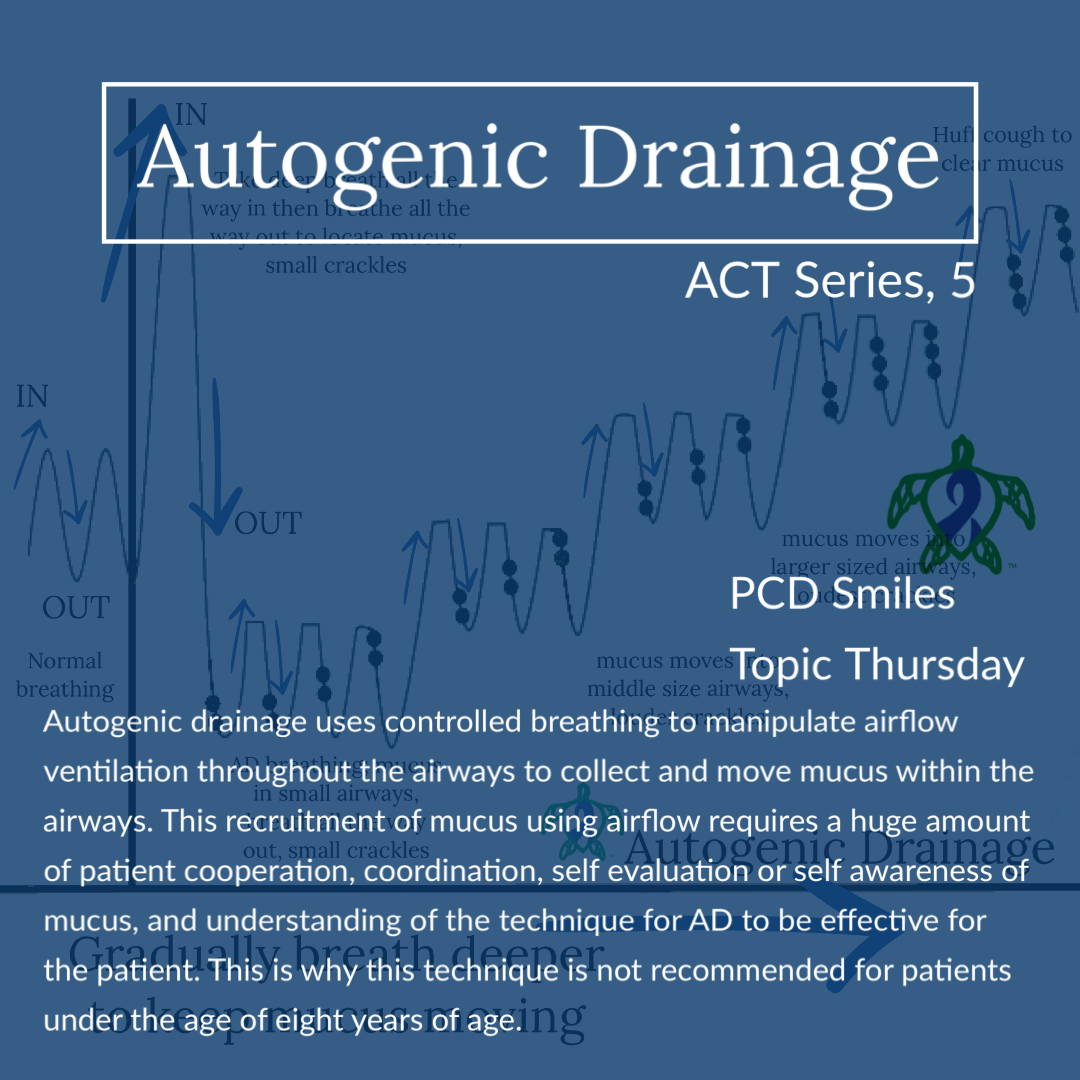
As we continue our deep dive into airway clearance our second breathing technique for airway clearance is autogenic drainage (AD). This technique was developed in 1967 by Jean Chevaillier and was first limited to only asthma before later being applied or rather approved for use in other airway diseases associated with overproduction of mucus in the bronchial tree. Autogenic drainage uses controlled breathing to manipulate airflow ventilation throughout the airways to collect and move mucus within the airways. This recruitment of mucus using airflow requires a huge amount of patient cooperation, coordination, self evaluation or self awareness of mucus, and understanding of the technique for AD to be effective for the patient. This is why this technique is not recommended for patients under the age of eight years of age. It also reinforces the need for proper training by a licensed respiratory therapist and should not be undertaken by simply reading about the technique on the internet or being coached by a non-professional. Autogenic drainage in it’s basic form means self drainage. It’s aims are to recruit the movement of mucus from the lower airways to the upper airways using different breathing frequencies without causing airway collapse that can happen during forced expiratory pressures of other airway clearance techniques.
AD is another popular ACT (airway clearance technique) method mainly for it’s cost effectiveness like seen in active cycle breathing. AD is widely used outside the United States with it being the fourth most prescribed ACT in Canada. Recent research within the CF (cystic fibrosis) population shows that children with CF see the most benefit using AD while adults with CF do not see as much improvement as the children do. This is hypothesized to be due to increased damage to airway walls, damage to mucociliary clearance, and increased viscosity of mucus in older CF patients. This is the subject of several current research studies. If these theories hold true the implications may need further research into how it extrapolates to PCD (primary ciliary dyskinesia) airway clearance recommendations.
AD can be done in conjunction with bronchodilator and mucolytic administration. So basically you can do AD while nebulizing bronchodilator solutions, like albuterol and mucolytic solutions, like hypertonic. AD can also be performed with certain PEP devices as directed by your licensed respiratory therapist. It’s important to note that there are contraindications for autogenic drainage such as recent thoracic or abdominal injury or surgical injury (basically while healing from chest and gut surgeries.) AD is also not appropriate for cognitively impaired individuals, patients who do not have moderate to large amounts of mucus because they won’t be able to hear the crackles, and patients diagnosed or suffering from gastric reflux.
Autogenic Drainage:
To perform safely, properly, and effectively it will take several sessions with a licensed respiratory therapist!
Find a comfortable upright or a slightly recumbent position while keeping your spine straight and lengthened. Do not slump or hunch. Remain in this position to help maintain lung ventilation. Refrain from coughing, suppress any need to cough, until the end of the cycle. The idea is to gather the mucus along the airways using the airflow from the breaths. Then cough at the end of the cycle to clear the mucus from the airways. Remain relaxed.
Normal Breathing
- Start with normal breathing in through the nose and out through the mouth for a few breaths.
- When ready proceed to the next step, Deep Breath.
Deep Breath
- When ready on the next breath take a gradual breath in through the nose all the way in.
- Pause for 2-3 seconds.
- Then gradually breathe out all the way through the mouth.
- Near the end of the breath there should be slight crackling sounds.
- Crackling indicates movement of mucus in the small airways.
- Resist need to cough (suppress coughing at this point.)
Step Breathing
- Take a gradual short breath in though the nose.
- Pause for 2-3 seconds.
- Then gradually breathe out a similar breath through the mouth.
- Crackles should be heard near the end of the gradual short exhale.
- Repeat 3-4 times.
- Crackles should get louder and come increasingly sooner in the exhale.
- This indicates the need to increase breath volume and move onto the next series of slight larger breaths.
- Each Step Breathing cycle should last between 2 - 3 minutes.
- STEP UP
- Take a slightly larger gradual breath in the nose.
- Pause for 2-3 seconds.
- Then gradually breathe out a similar breath through the mouth.
- Should hear crackles near the end of the gradual exhale.
- Repeat 3-4 times.
- Crackles should get louder and come increasingly sooner in the exhale.
- This indicates the need to increase breath volume and move on to a series of slightly larger breaths.
- Each Step Breathing cycle should last between 2 - 3 minutes.
- Repeat STEP UP up to three times while suppressing cough.
- Third time move onto coughing.
Huffing
- Breathe out (exhaling) through an open mouth and throat and not coughing.
- Squeezing air out through your open throat and mouth as if steaming up a mirror.
- Always follow huffing by breathing control.
Coughing
- If you can clear your mucus by huffing then you do not need to cough.
- Only cough if mucus can be cleared easily.
- After three coughs return to the beginning of the cycle with normal breathing.
**Repeat the cycle until you feel that your huff or cough is not producing any mucus, or for up to twenty minutes depending on your respiratory therapist.

It was once thought in primary ciliary dyskinesia that coughing and breathing techniques like autogenic drainage were enough to compensate for the lack of mucociliary clearance seen in PCD. Recent research has now shown not only is this not the case, but that there is a sensory component to motile cilia. When motile cilia are under stress they signal the CFTR channel to do its job and send more hydration to the mucus to thin the mucus in the airways. With defective motile cilia in PCD the CFTR never gets the signal, because the cilia are broken at the cellular level, which is thought why mucus viscosity seen in PCD is similar to that of the mucus viscosity seen in cystic fibrosis (CF). This could highlight why more aggressive airway clearance techniques are needed in PCD, especially as the destruction caused by PCD progresses. With some people with PCD needing aggressive ACTs in infancy. In any case as research in PCD advances so will our understanding of cilia and it’s roles in clearing the airway. Learning the ins and outs of airway clearance techniques will remain an essential part of doing life with primary ciliary dyskinesia. We hope that you join us next week for part six of our series on airway clearance techniques.
Be sure to join us next week for another Topic Thursday.
Join our Facebook group Turtle Talk Café today, click here.
We have several ways that you can donate to PCD Smiles;
- Visit Smile E. Turtle's Amazon Wishlist
- For more information on how you can donate, please visit our "Donation" page to check out our "Do & Don't policies.
- Or sponsor a PCD Smiles cheer package today!
- To shop for your “Official” turtle care ribbon gear today, visit PCD Style or Smile E. Cove
Thank you for your consideration!
***Please speak to your respiratory therapist or your PCD medical team before commencing any new treatment. DO NOT start using a device, or technique, on this website if you have not discussed this with your PCD team first.***