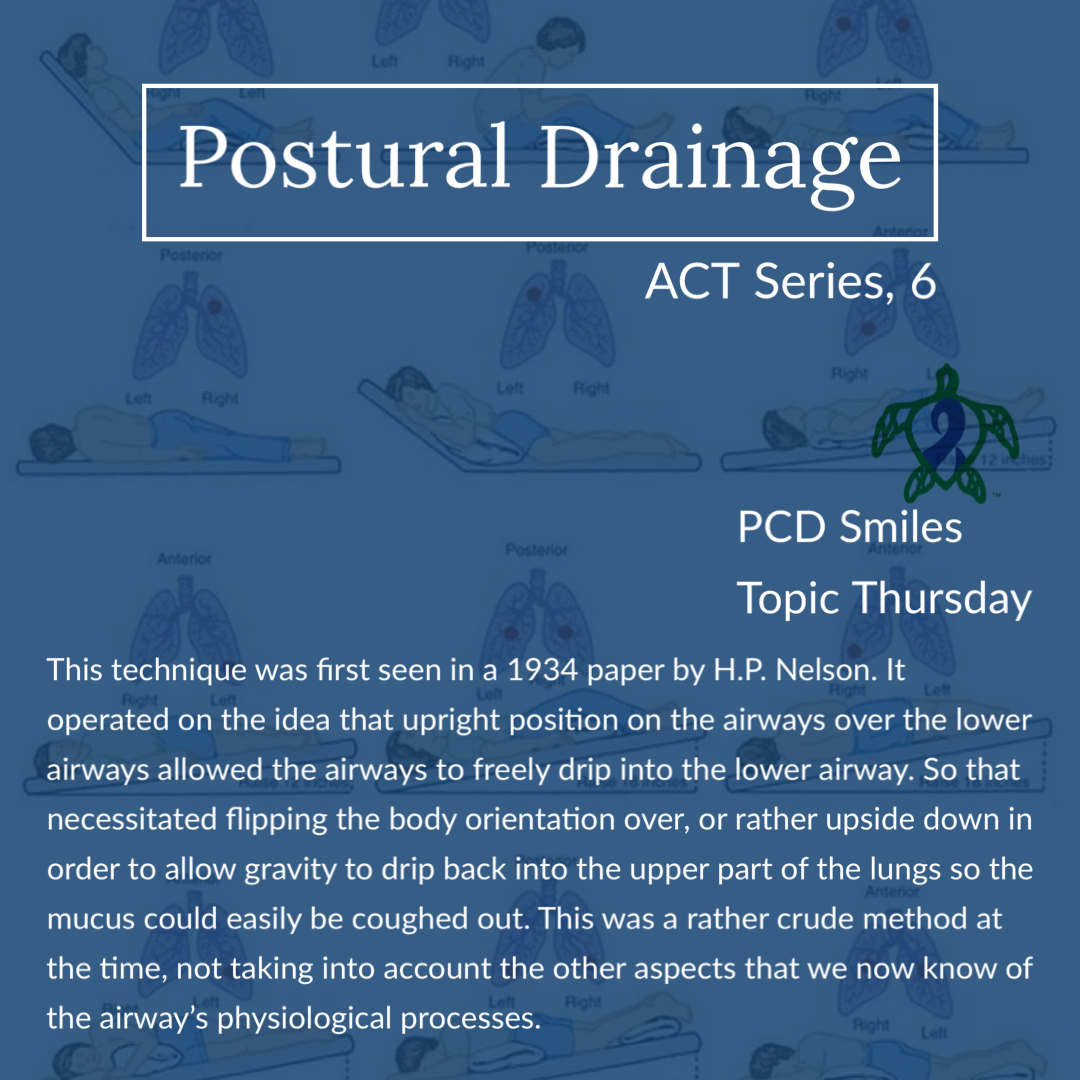
As we continue our deep dive into airway clearance the first technique for airway clearance was postural drainage (PD). This technique was first seen in a 1934 paper by H.P. Nelson. It operated on the idea that the upright position of the airways over the lower airways allowed the airways to freely drip into the lower airway. So that necessitated flipping the body orientation over, or rather upside down in order to allow gravity to drip back into the upper part of the lungs so the mucus could easily be coughed out. This was a rather crude method at the time, not taking into account the other aspects that we now know of the airway’s physiological processes. However this method of airway clearance was widely used from the 1930s well into the mid 1980s when researchers made some startling discoveries in the quest to aid the cystic fibrosis (CF) community in finding better treatments for CF patients to extend their life expectancy and improve their overall quality of life. As time advances, so does our understanding of things we research, and therefore we must be ready to advance into the future using current knowledge. As a good friend of mine always says, “We can only operate with the knowledge that we have at the time.”
Postural drainage (PD) started out in the beginning as just that, positioning the patient in multiple positions for extended periods of time to allow the mucus from the higher positioned section to drain towards the bronchial tree. These positions where held up to thirty minutes each at the beginning of the practice of PD. By the 1970s the time was cut down to three to five minutes before transitioning the patient to the next PD position. Recent studies have shown to be effective PD positions need to be held for upwards of one hour each position, which do not make them very convenient for the little benefit that PD has recently been shown to provide in mucociliary clearance disorders given other devices and techniques currently available. PD was done at the direction of a licensed respiratory therapist while inpatient at a care facility. The CF community parents where given training by a respiratory therapist to preform these maneuvers at home. Somewhere in the late 1960s to 1970s depending on the geographical location percussion and vibration where added into the mix of PD. Next week’s ACT Series will cover PD&P (postural drainage and percussion, also known as chest physiotherapy in most countries).
PD was recommended for cystic fibrosis, bronchiectasis, atelectasis, spinal cord injuries, and other patients who have thick sticky and hard to move mucus for varying reasons. What was once the gold standard of treatment for these conditions has been retired by most facilities and clinics due to lack of consistent coordination of standards, aging respiratory population (most notably the CF population) that makes this unsustainable in care centers in place of more convenient and modernized devices that a patient can perform themselves, by themselves. As well as several studies showing more and more contraindications of PD in subsets of patients than the realized benefits of PD in those subsets of patients. Also we now have a greater understanding of gravity assisted drainage than was available in the 1930s which shows that drainage is more about ventilation than it is actually about gravity doing the work. If you can’t get air behind the mucus then the mucus won’t move. Getting ventilation or rather air behind mucus is essential to moving mucus along the airways. Studies in the early 2000’s have shown that newer PEP devices used in conjunction with PD actually produce greater mucus clearance from ancillary airways than the higher airway in a given position. So basically if the right lower lobe is positioned higher for targeted gravity drainage, the left lower lobe gets better mucus drainage than the intended right lower lobe that is positioned higher. So the adjacent airways get better clearance, which points to ventilation being the driving force behind airway drainage. This seems supported by an article in 2002 by Fink J.B. in Respiratory Care that stated that gravity is not a physiological mechanism for transporting mucus but is important for lung function (it has an effect on ventilation, perfusion, and lymphatic drainage.) There are also several studies pointing to increased bronchiectasis progression or rather faster progression of a patient’s bronchiectasis due to PD, this is the subject of controversy among various professional practitioners, mainly physical therapist who try to offer PD to their clients. However most mucociliary clearance medical professionals advise against PD especially in an inclined position (head lower than the heart position), especially to their patients with forceful coughing like seen in primary ciliary dyskinesia (PCD) and CF. The American Association of Respiratory Care around about 2018 actually retired it’s Clinical Practice Guidelines on postural drainage for many of these stated reasons.
The list of postural drainage contraindications continues to grow. PD is contraindicated but not limited to patients with shunts, pneumothorax, atelectasis, recent head surgery or trauma, inter cranial pressure issues, blood pressure issues, blood clotting disorders, aneurysms, head or neck injury, hemorrhages, active airway bleeds, aged, confused, cognitively impaired, distended abdomen, pacemakers, newly installed or repaired implants including pacemakers, bronchospasms, pulmonary TB, pulmonary NTM, open wounds, open burns, osteoporosis, chest wall pain complaints, arrhythmias, emphysema, esophageal surgery, and the list goes on. Possible complications of PD include but are not limited to aspiration, bronchospasm, vomiting, headaches, hypoxia, pulmonary hemorrhage, increased inter cranial pressures, and pain or injury to chest wall, chest muscles, ribs, and the airways. PD is not an effective method of airway clearance in patients who do not produce a lot of mucus and is therefore not recommended for patients who don’t cough up much mucus. The supine position (laying face up) for extended period of time can allow the mucus to pool in various spots of the lungs, and the upper side of the airway to dry out exposing the patient to infection and obstruction. Laying prone (laying face down) helps ventilation, ancillary airway ventilation and recruitment, and helps improve tidal volume of the lungs. Side lying increases overall lung ventilation, and increases the gas exchange in the dependent lung; the lung closest to say the bed. PCD patients are counseled to change their position frequently when laying down to help prevent mucus pooling and thereby avoiding increased infections.
It was once thought in primary ciliary dyskinesia that coughing, breathing, and positioning techniques like postural drainage were enough to compensate for the lack of mucociliary clearance seen in PCD. Recent research has now shown not only is this not the case, but that there is a sensory component to motile cilia. When motile cilia are under stress they signal the CFTR channel to do its job and send more hydration to the mucus to thin the mucus in the airways. With defective motile cilia in PCD the CFTR never gets the signal, because the cilia are broken at the cellular level, which is thought why mucus viscosity seen in PCD is similar to that of the mucus viscosity seen in cystic fibrosis (CF). This could highlight why more aggressive airway clearance techniques are needed in PCD, especially as the destruction caused by PCD progresses. With some people with PCD needing aggressive ACTs in infancy. In any case as research in PCD advances so will our understanding of cilia and it’s roles in clearing the airway. Learning the ins and outs of airway clearance techniques will remain an essential part of doing life with primary ciliary dyskinesia. We hope that you join us next week for part seven of our series on airway clearance techniques.
Be sure to join us next week for another Topic Thursday.
Join our Facebook group Turtle Talk Café today, click here.
We have several ways that you can donate to PCD Smiles;
- Visit Smile E. Turtle's Amazon Wishlist
- For more information on how you can donate, please visit our "Donation" page to check out our "Do & Don't policies.
- Or sponsor a PCD Smiles cheer package today!
- To shop for your “Official” turtle care ribbon gear today, visit PCD Style or Smile E. Cove
Thank you for your consideration!
***Please speak to your respiratory therapist or your PCD medical team before commencing any new treatment. DO NOT start using a device, or technique, on this website if you have not discussed this with your PCD team first.***